Leading the Way to Precision Health
Empower Patients and Clients with Targeted Plans and Effective Outcomes
The world has shifted and today 8 out of 10 people consider wellness the top priority in their lives. With Metabolic Code® you meet this demand by helping them determine how far away they are from being truly healthy and giving them a path to vitality.


The Challenge
Despite their desire, individuals find themselves navigating a complex and confusing journey to a healthier life.
Many solutions are either too general and not tailored to meet their individual needs, or fail to focus on a systems approach to solve systemic issues.
Metabolic Code® leverages a proprietary 40,000-point Bayesian Model algorithm to empower your practice with a platform which gives clients answers to questions they really want to know:
- Where is my health today?
- What does it mean?
- What do I do about it?
Rich History & Renowned Credibility
The Birth of Metabolic Code®
Founded by a team of leading experts in integrative medicine with over 100 years of collective experience, Metabolic Code® provides unparalleled knowledge for patients and clients. Developed by Jim LaValle, RPh, CCN, DHM, DHPh, renowned clinical pharmacist, author, and health expert with over 40 years of experience in integrative and precision medicine. And internationally recognized pioneer, scientist, clinician and educator in Integrative and Metabolic Medicine, Dr. Andrew Heyman, M.D., MHSA who currently serves the Medical Director of Integrative Medicine at The George Washington University.
- Leads the next generation of healthcare practitioners through the American Academy of Anti-Aging Medicine (A4M), the largest private education organization in the world in Anti-aging, Functional and Integrative Medicine.
- LaValle is also the clinical co-chair at A4M, Chair of the International Peptide Society and Chief Science Officer at LIFE TIME (NYSE: LTH).
- Heyman is considered a world expert in Biotoxin Illness and Chronic Inflammatory Response Syndrome (CIRS) and triple Board certified in Family Medicine, Integrative Medicine and Anti-Aging and Regenerative Medicine.
- Metabolic Code® has been reviewed and approved by the Curriculum Committee at the George Washington University, serving as their capstone course for a Masters Degree in Integrative Medicine.
- Metabolic Code® also includes a team of licensed and practicing dietitians who have been at the forefront of dietary guidance for over 3 decades.


1985
Jim develops the first “food tagging system” for Kroger and co-authors the “Consumer Guide to Low Cholesterol Shopping.”
1985
Jim begins a world-leading clinic, implementing various disciplines of natural medicine into an integrative care model for thousands of patients.
1988
Jim begins leading integrative medicine forward. Designs over 200 nutritional products and serves as a leading consultant around the world.
1997
After extensive years of clinical practice and real world application, the architecture for the Metabolic Code® is conceptualized.
2004
Jim publishes the best-selling book Cracking the Metabolic Code® which is a cornerstone text for health professionals worldwide.
2008
The first algorithm model is designed and over the next four years is modeled, refined, and validated using clinical endpoints.
2016
The Metabolic Code® is selected as the foundation for the capstone course in integrative medicine at George Washington University.
2024
Metabolic Code® is a renowned platform leveraged by U.S Special Operations Command, LIFE TIME, and Evexias™ Health Solutions, a network of 5,000 clinics.

Enhance Your Practice
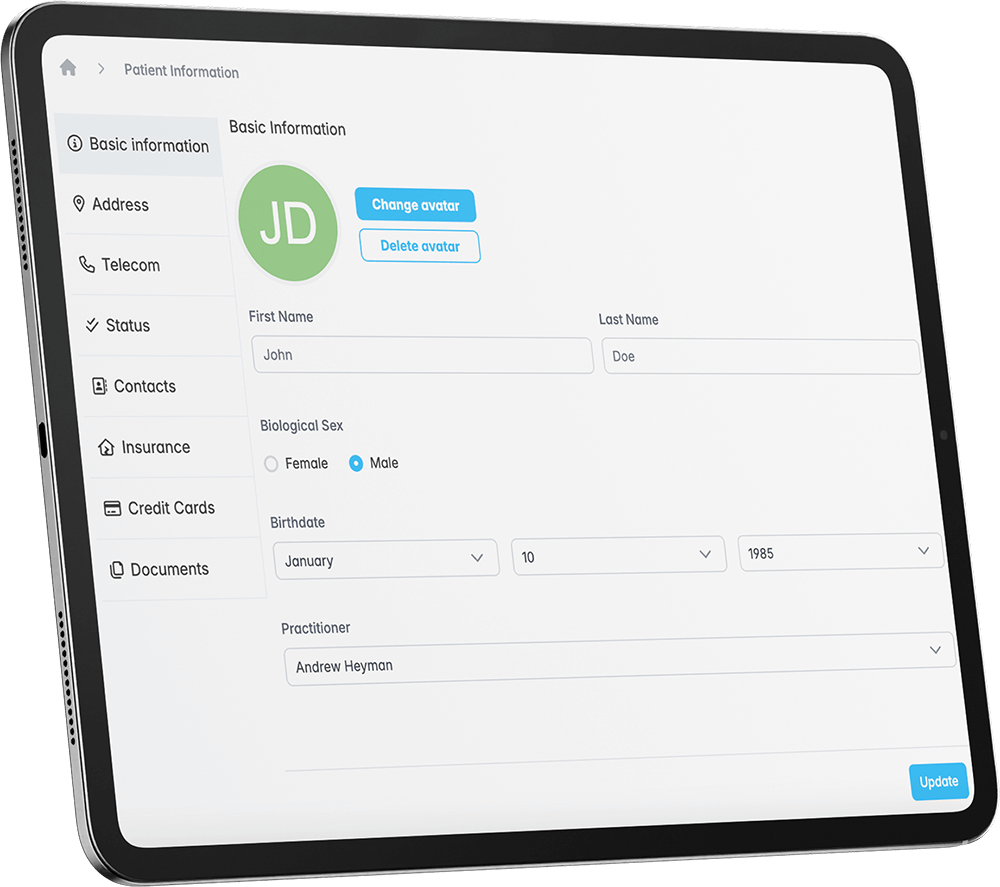
With Metabolic Code® you can provide your patients with personal wellness programs tailored to meet their needs.
Our programs are based on a systems biology approach and processed through our proprietary technology which continuously adapts and refines recommendations as new data is added.
Patient expectations have changed. With our cloud-based software you can:
- Improve clinical outcomes through targeted patient plans
- Improve engagement by tracking progress
- Increase revenue through improved adherence
- Deliver effective results through personalized lifestyle plans
Key Benefits
Take your practice to the next level with...

Systems-Based
Programs & Protocols
- Resolve systemic issues related to the whole-person health of each patient.
- Receive exclusive pricing for patient labs and advanced diagnostics.
- Access to comprehensive tools and training to implement proven precision lifestyle programs into your practice.
Metabolic Code®
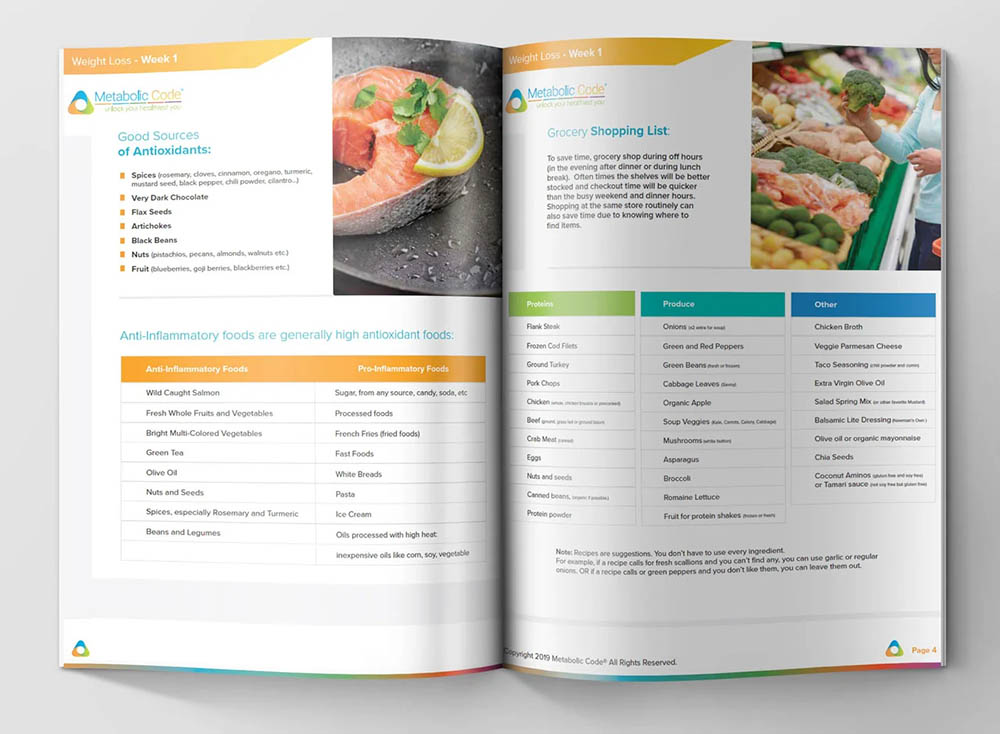
Knowledge Library
- Access to the Metabolic Code® Library which includes training and education materials, sales collateral, diet plans, lifestyle programs and so much more.
- New and refreshed product and nutrient monographs.
- Deep-dive webinars, TRIAD training and case reviews.

Exclusive
Products
- Unique formulations to address the needs of the 5 TRIADS.
- 3rd party tested, no harsh chemicals are used during extraction, and we use only natural fillers, binders, and no harsh synthetic binders or dyes in any of our products.
- Receive access to top-tier network of compounded pharmacies.
- Fully referenced professional monographs for each product.
How It Works
How to become a Metabolic Code® Practitioner.
1 Fill Out The Form
Please be sure to enter the official email that you would like to use for your account as this will be the email address we use for all correspondence. If we have any questions related to your application, a representative may call you to assist in completing your account setup.
2 Get Approved
Once your application has been approved, your Metabolic Code® account will be created, providing you access to the Metabolic Code® Library and supplement store. You will also be emailed login details for access to the Metabolic Code® Assessment Tool.
3 Get Onboarded
After registration you will be given access to training materials in the Metabolic Code® Library and will also be able to schedule a session with one of our onboarding specialists. To place lab orders through the Metabolic Code® platform, we require that your license allows for lab ordering privileges in the states where you practice.
Pricing
Metabolic Code®
Membership and SaaS Subscription
$349
per month
One (1) Authorized User / One (1) Location
Additional Features
Additional Practitioners / Locations
* A subscription is required for each practicing provider per location.
Contact for Pricing
Metabolic Code® Reports
$10 per report
Metabolic Code® Approved Supplements
* Wholesale pricing offered directly through Metabolic Code Website.
Metabolic Code® TRIADS™
Precision health begins
with the Triads™.
Our personalized evaluation program not only creates a precise plan of action for people to live and feel better, it also tracks progress with real world data. The Metabolic Code® is based on 40 years of clinical research and application. It relies on the process of measuring a person’s unique metabolic signature, called metabotyping. Like taking an internal fingerprint, the assessment process uncovers 5 domains of physiologic functioning we call TRIADS™. The Metabolic Code® TRIAD™ Metaflammation Scores (TMS) represent how metabolically efficient each domain is functioning.
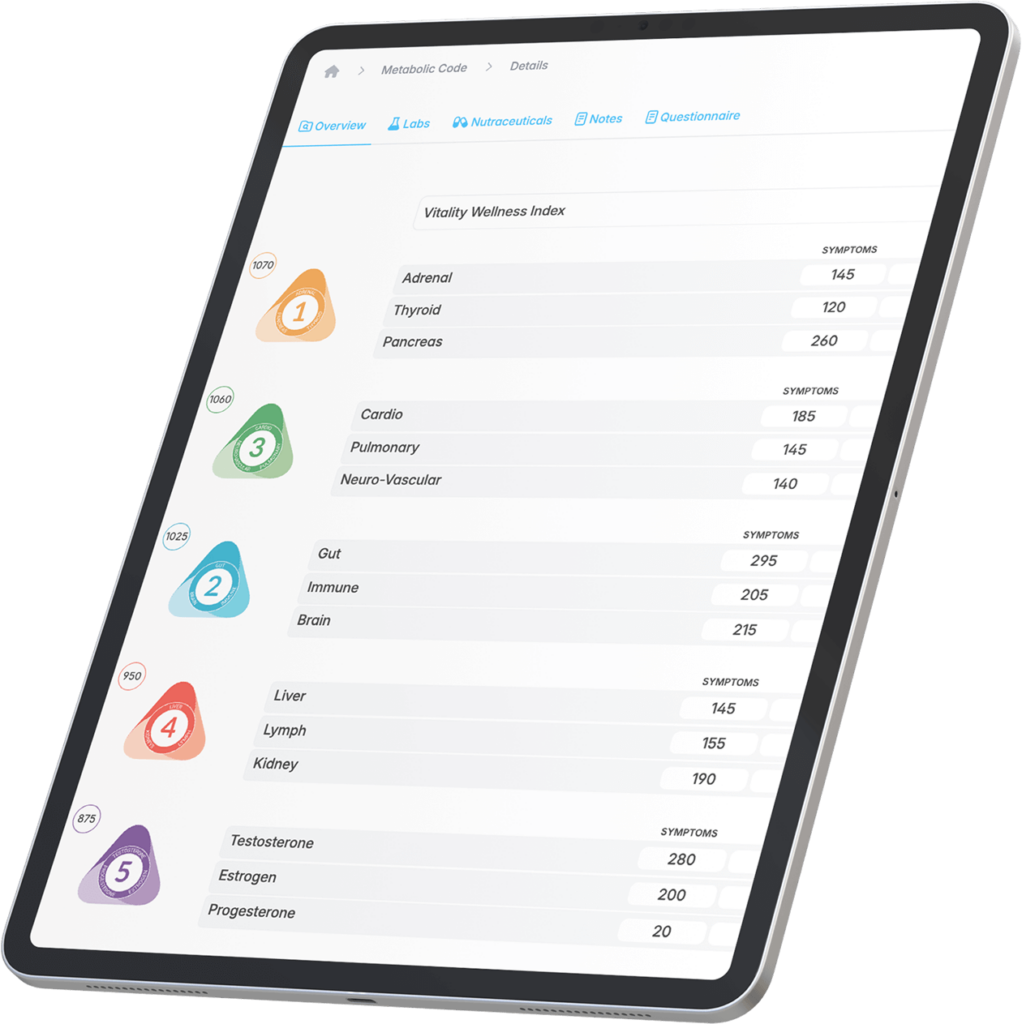
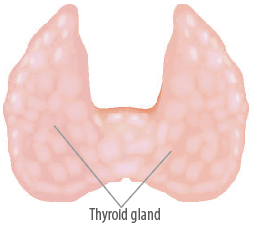
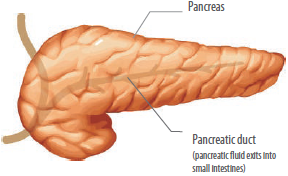
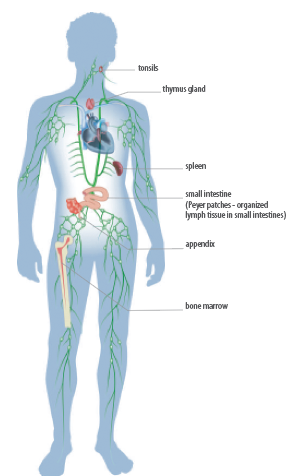
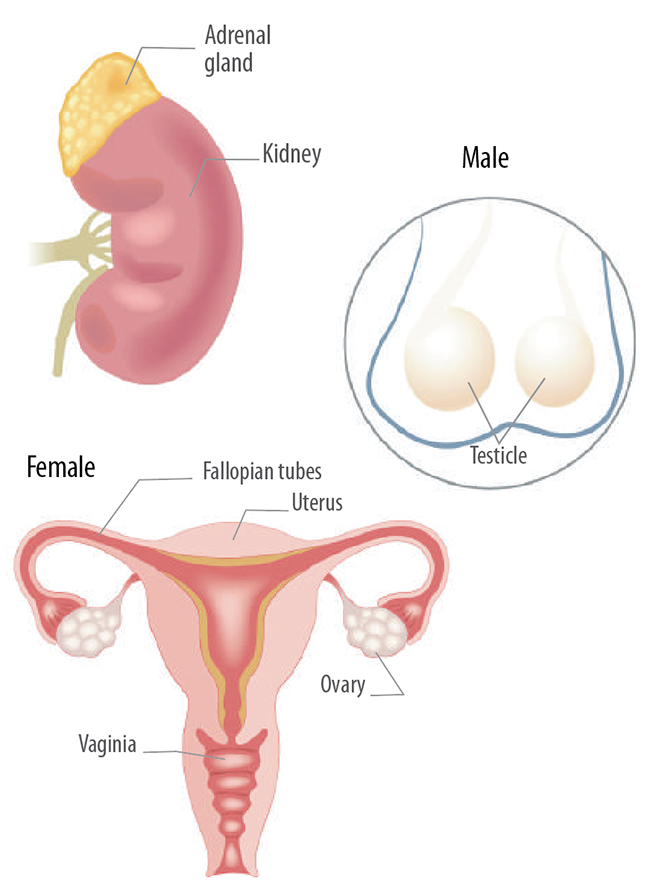
Triad 1
Energy
Adrenal • Thyroid
• Pancreas
Discover the symbiotic relationship between important hormones that influence energy production within the body.

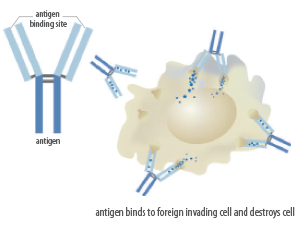
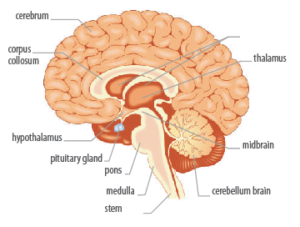
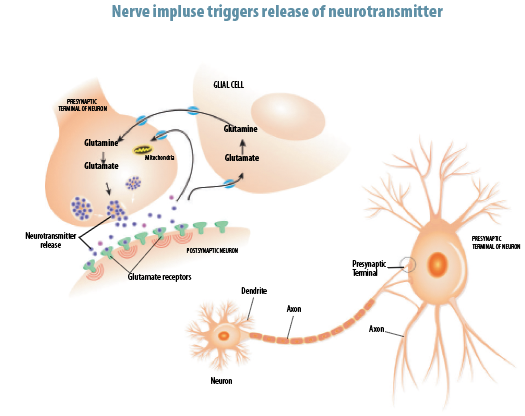
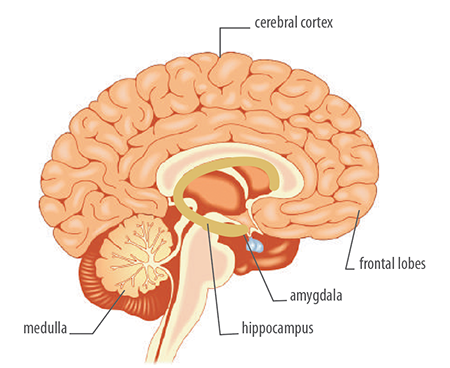
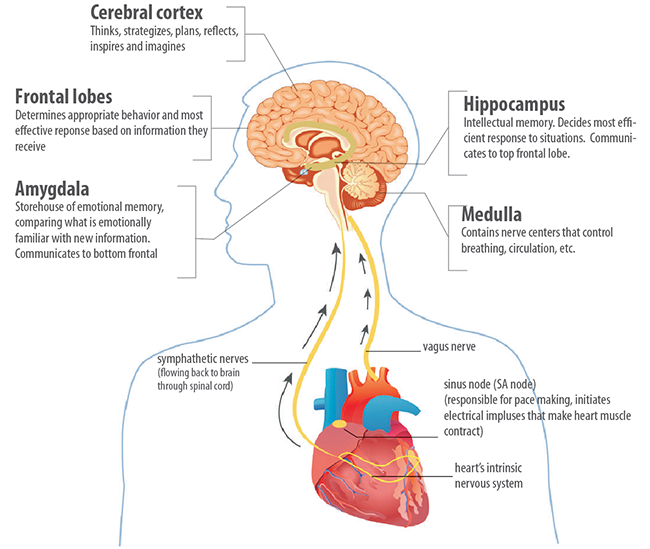
Triad 2
Resiliency
Gut • Immune
• Brain
These interrelated, intelligent systems are critical to nutritional, immunologic, and mental health.

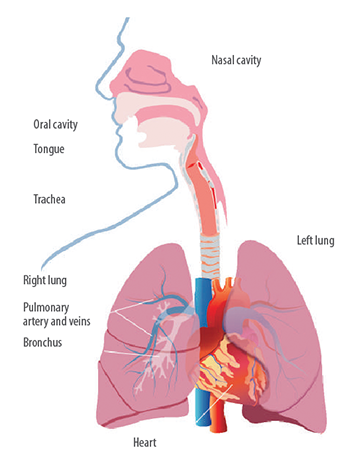
Triad 3
Endurance
Cardio • Pulmonary
• Neuro-Vascular
Encapsulates the multilayered connections between of the mind, brain, cardiovascular tree, and respiratory cycle.

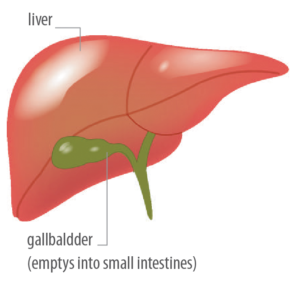
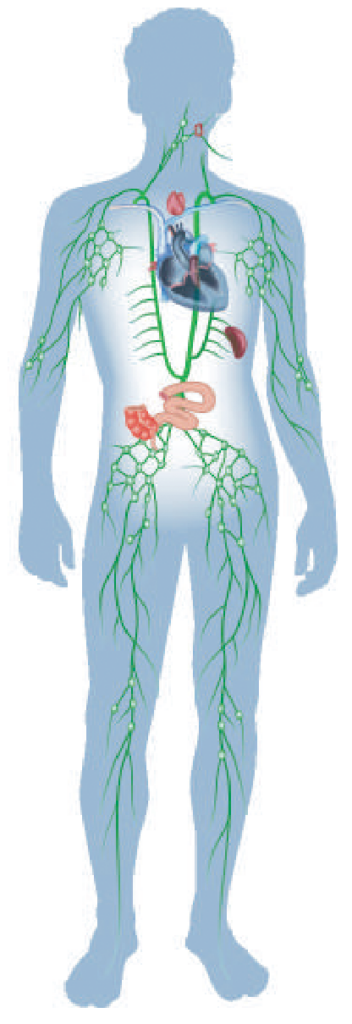
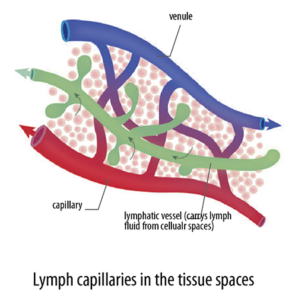
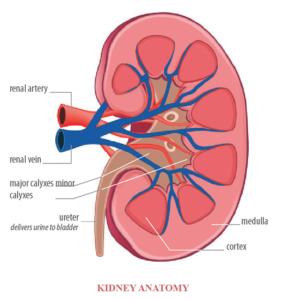
Triad 4
Detoxification
Liver • Lymph
• Kidneys
Promotes elimination of toxic waste through proper detoxification processes.

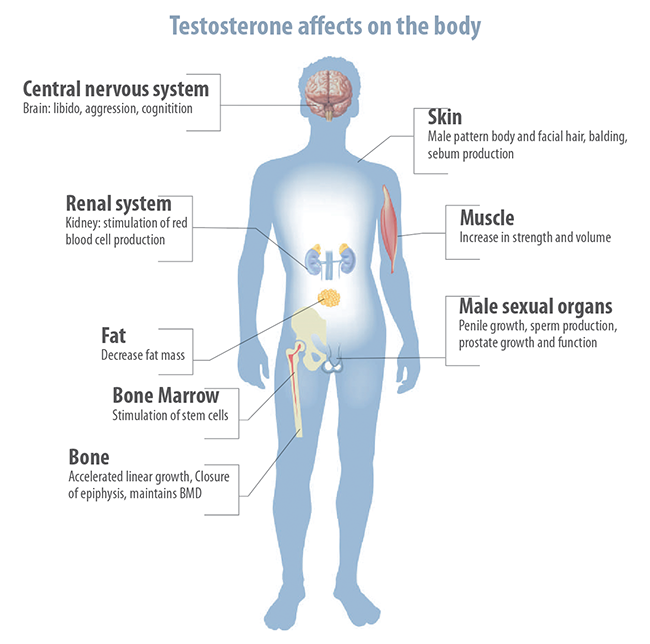
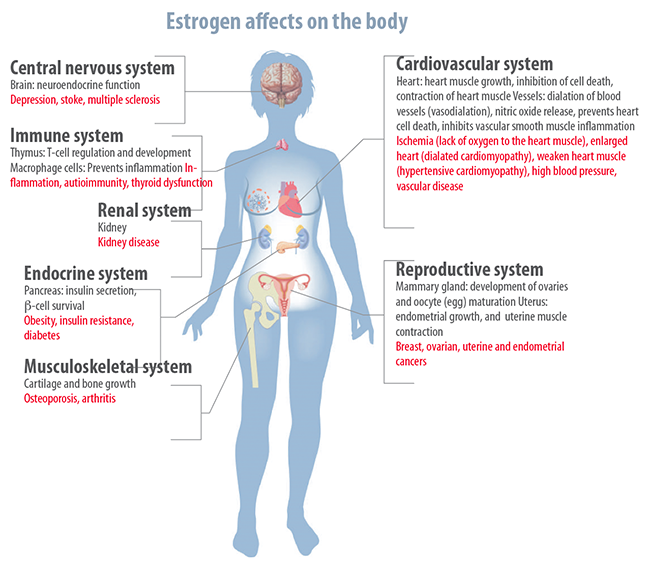
Triad 5
Potency
Testosterone • Estrogen • Progesterone
Finds balance across the life cycle through proper functioning of reproductive hormones.

Unlock Your Healthiest You™
Get Your Personalized Program
Experience what so many others have done to rapidly improve their health and vitality long-term. Get your personalized Metabolic Code® Report and find out what your metabolic deficiencies are while learning how to correct them. We have lifestyle programs created for people with all types of goals and dietary needs. Ask your healthcare practitioner or fitness coach about getting your own Metabolic Code® Program.
Exclusive Supplements
Quality products you can trust.
High impact formulations that are safe, fully transparent, and utilize the raw materials that are evidence-based in therapeutic amounts.

Apply to the Metabolic Code® today to begin bringing longevity, vitality and personal wellness into your practice.
Begin generating personalized Metabolic Code® reports, get exclusive access to the Metabolic Code® supplement store, and unlock the resource & education library.